Big Latch On Blog
Welcome to the Big Latch On blog! Here you will find information about different ways to feed pēpi. It is important that all parents feel welcome to celebrate their feeding journey and the village that supports them, whatever this looks like, as each whānau and pēpi are unique. We hope that you will come together to join us in celebrating the Big Latch On to #feedyourway.
What is donor milk?
Sometimes breastfeeding doesn’t go to plan and a parent isn’t able to make enough breastmilk for their pēpi (baby). Where available, donated breastmilk (human milk, also known as donor milk) can be used, rather than formula. Premature babies especially need human milk for the immune protection and growth factors. The World Health Organisation recommends the use of donor human milk, if mother’s own milk is insufficient or unavailable.
Milk banks, such as the Whāngai Ora Milk Bank, were established to collect and distribute safe donor milk for such occasions. The milk is screened, pasteurised (heat treated) and tested to make it the safest option for pēpi (as an alternative to a māmā’s own milk).
Donor milk can be fed to pēpi via a SNS (Supplementary Nursing System), feeding tube, bottle, cup or syringe.
Donor milk for vulnerable babies
In a perfect world, there would be milk banks in all regions. We are aware of the following milk banks: Whangārei Hospital’s Te Kotuku Maternity Unit, MidCentral (Whāngai Ora Milk Bank), Wellington (Pātaka Miraka Mothers Milk Bank), Christchurch (Human Milk Bank — Canterbury) and Nelson/Blenheim Hospital Maternity Units. These milk banks are primarily used for feeding premature or sick babies in Neonatal Units (NICU) and most referrals need to come from a midwife or other health professional. The aim of milk banking is that it is a short-term gift to help māmā establish their own supply’s, with the help of a lactation consultant.
Becoming a milk donor
Donating human milk is one of the most amazing gifts you could give! If you have milk to share with vulnerable babies, please contact your local milk bank to donate your breastmilk. All donors must undergo blood tests and complete a health and lifestyle screening questionnaire to ensure the safety of the milk (for example, questions about types of medications, alcohol and tobacco use and risk of blood-borne illnesses). Donors’ privacy is very important; therefore, they remain anonymous to the recipients of their donated milk.
Staying safe
Donated breastmilk from somewhere other than a milk bank, usually won’t be pasteurised to destroy bacteria and viruses. It may also contain traces of medication that the donor is taking. As a precaution, always check the health status of a donor and make sure the milk has been collected in a safe and hygienic way. Always seek advice from your midwife or Well Child Tamariki Ora nurse before using donor milk.
Feeding in public
Breastfeeding is a great way to feed pēpi when you’re out. It’s free, fresh, and requires no preparation! Being able to feed anywhere at any time will also help you maintain a good milk supply. While breastfeeding your baby is the most natural thing, it can often take some time to build your confidence to feed in public.
Here are some tips from other parents:
✨ Take a friend – to build your confidence, you might like to go out with friends or whānau who are comfortable feeding in public.
✨ Know your rights – while most people are completely fine with parents feeding in public, it is good to know that Under the Human Rights Act, it’s illegal for someone to stop you from breastfeeding or expressing milk in public. If you’re worried someone might make a comment, you might like to think about what you might say. You could quote your legal rights, or it could be as simple as “We’re happy feeding here, thank you”.
✨ Dress for the occasion—while you can find clothing specially made for breastfeeding, layers and tops that are easy to pull down or up also work well. Some parents may feel more comfortable wearing a scarf or muslin cloth over their chest while feeding. You do you!
✨ Food on the go – you can breastfeed your baby in most baby slings and carriers, giving you a bit of privacy and freeing your hands to enjoy a drink (or chase a toddler) while you’re out.
✨ Lookout for a ‘He Wāhi Haumaru’ (Breastfeeding Welcome here) sign – lots of cafés and stores will display these to show they are a breastfeeding-friendly space.
What helped you to feel confident breastfeeding in public?
Can you feed for too long?
No! There’s no limit for how long you should breastfeed your child – that’s a decision that only you and your child can make. And we’re all about celebrating your individual feeding journey!
Did you know that the Ministry of Health recommends breastfeeding until at least 2 years of age, and the natural weaning age for humans is 2-7 years old, with most toddlers naturally weaning between 2-4 years old.
Your breastmilk is still nutritious no matter how long you feed for, and continues to be a good source of energy, protein and vitamins beyond 12 months, not to mention all the helpful antibodies and immune factors. Feeding an older child also provides lots of benefits including protection from illness (meaning less sickness and shorter illness when they do get sick), boosts brain development in toddlers and provides ongoing comfort – a superpower when needing to soothe your child.
Of course, sometimes it’s not possible for everyone to feed for as long as they had hoped for (with many tamariki deciding for us!). On the other hand, sometimes we can end up feeding for longer that we had planned or wanted to. However long you’ve feed your child for, we think you are amazing and every drop counts!
Leaking milk
Leaking breastmilk is totally normal and very common! It can happen before you give birth and is most common in the early days as your breasts are adjusting to feeding. This can happen while you are feeding on one side, with the other side leaking, or when you’re not feeding at all (often a baby’s cry can trigger a let-down).
Wearing breast pads can help to absorb this milk (and save you having to change your shirt multiple times a day). Some parents like to refrigerate or freeze reusable breast pads that contain collected milk and use these in a warm bath for pēpi. Wearing darker clothes can help to camouflage milk marks and at nighttime you may like to use a mattress protector or towel underneath you.
Some parents use a silicone milk catcher either at feeds or between feeds to collect milk. It’s important to use these with caution as continuous suction can cause an over-supply of milk, which may cause other issues such as mastitis.
Leaking milk usually lessens or stops as pēpi gets older, although some parents may find they continue to leak, especially during the let-down reflex. Did you experience leaking milk?
What is Tandem Feeding?
Tandem feeding is feeding two children of different ages at the same time. For example, feeding a baby and their older sibling. Some māmā or parents will feed both tamariki at the same time, whilst others will take turns feeding one at a time throughout the day. Parents of twins (or multiples) may also choose to tandem feed, by feeding both babies at the same time.
Tandem feeding is a really beautiful and natural way of continuing to breastfeed an older child when a new baby comes along. Your body adapts to produce enough breastmilk for both children – how incredible! Some tandem feeding parents choose to have one breast available to each child, whilst others choose to offer both breasts to both children. It’s important to offer the breast to your newborn first, to ensure they are getting all the immune-boosting colostrum they need. You may find that you need to feed your children separately if your newborn isn’t full after just one breast and is needing the second breast.
What is Chestfeeding?
While most people use the term “breast feeding,” some people prefer the term “chest feeding,” to describe how they feed their baby from their bodies. While anatomically speaking both men and women have breast tissue, due to the gendered connotations of the word ‘breast,’ it’s important to check with the person in your care what language is most affirming for them.
Anyone can feed a baby from their body and whilst most cisgender men would choose not to induce lactation due the dysphoria they would feel at breast tissue growth, it is possible. Many transgender and non-binary parents will induce lactation to feed their baby. They can also co-feed their pēpi alongside their partner(s). Inducing lactation if you weren’t the parent who was pregnant involves taking oral contraceptives, followed by an additional drug called domperidone. Domperidone is primarily used as an anti-nausea medication, but also causes lactation. It is also given to cisgender women with low supply to increase their milk supply. Alongside the drugs needed to induce lactation, the parent will need to pump and express milk mimicking that of a newborn baby. This isn’t the right choice for every parent and is not the only way to bond with a baby.
People who have had top surgery may also still be able to lactate, but this will depend on how many, if any, milk ducts have been left behind during surgery. Not everyone who has had top surgery will want to or can feed a baby from their body but it is an option for those who wish to. Some transgender and non-binary parents may choose to express milk instead of, or in addition to feeding their baby at their chest.
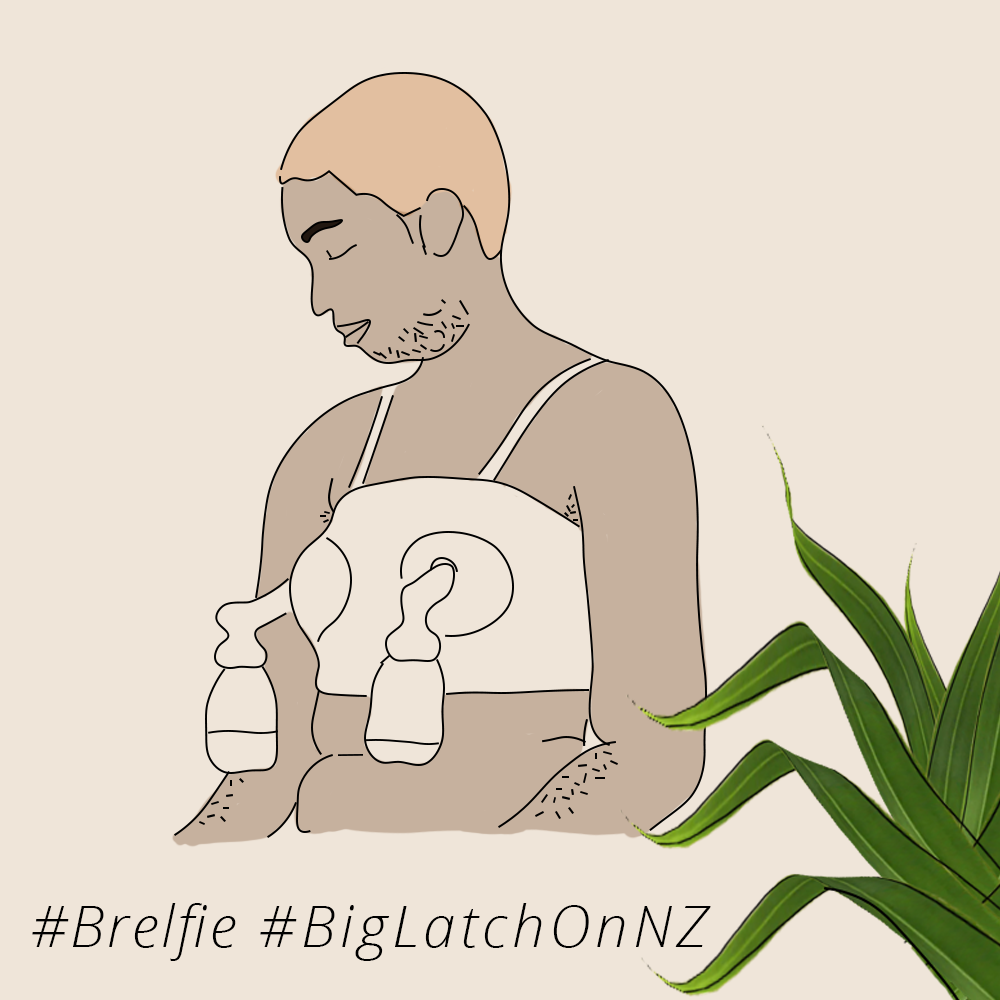
Feeding with a Supplemental Nursing System
A supplemental nursing system (or SNS) is a way of feeding milk to your baby if you’re co feeding, adding top ups for medical reasons or aren’t able to produce enough or any breastmilk.
There are lots of benefits for a pēpi to latch to the breast or nipple that isn’t just getting milk. Using an SNS means that pēpi gets all the benefits of latching to the nipple, whilst being skin-to-skin, and being fed human or formula milk. SNS works by using a bottle, container or syringe to hold expressed breastmilk, donor milk, or formula and a small thin flexible tube that sits in line with the nipple so that as baby sucks on the nipple, they draw milk from the bottle, through the tube, and into their mouth.
Using an SNS allows the baby to suckle which can help to produce more breastmilk if the feeding parent is lactating; and it can help the baby to develop their oral sucking skills.
People with low supply or who have undergone a mastectomy, as well as people who have had top surgery, are some of the many people who may use an SNS to feed their baby.