Menopause happens when your menstrual cycle stops. Once menopause begins, the ovaries produce lower levels of the reproductive hormones oestrogen and progesterone. The average age for menopause in New Zealand is 51.5 years but it can occur anytime between the ages of 42 and 56. If you haven’t had your period for 12 months, you may be beginning menopause.
Perimenopause is the period of five or so years up to the last period when menstruation becomes irregular or occurs less often and eventually ceases. During this time, hormone levels change and you may begin to experience changes in your body. After menopause your body achieves a new hormonal balance, however during the transition phase, the changes in hormone levels can have a number of effects on women and people with uteruses.
Symptoms
Experiences of menopause vary among individual people and different cultures. How menopause affects individual people is influenced by biological and social factors, including genetics, physical and mental health, diet, lifestyle, and social and cultural attitudes toward older women.
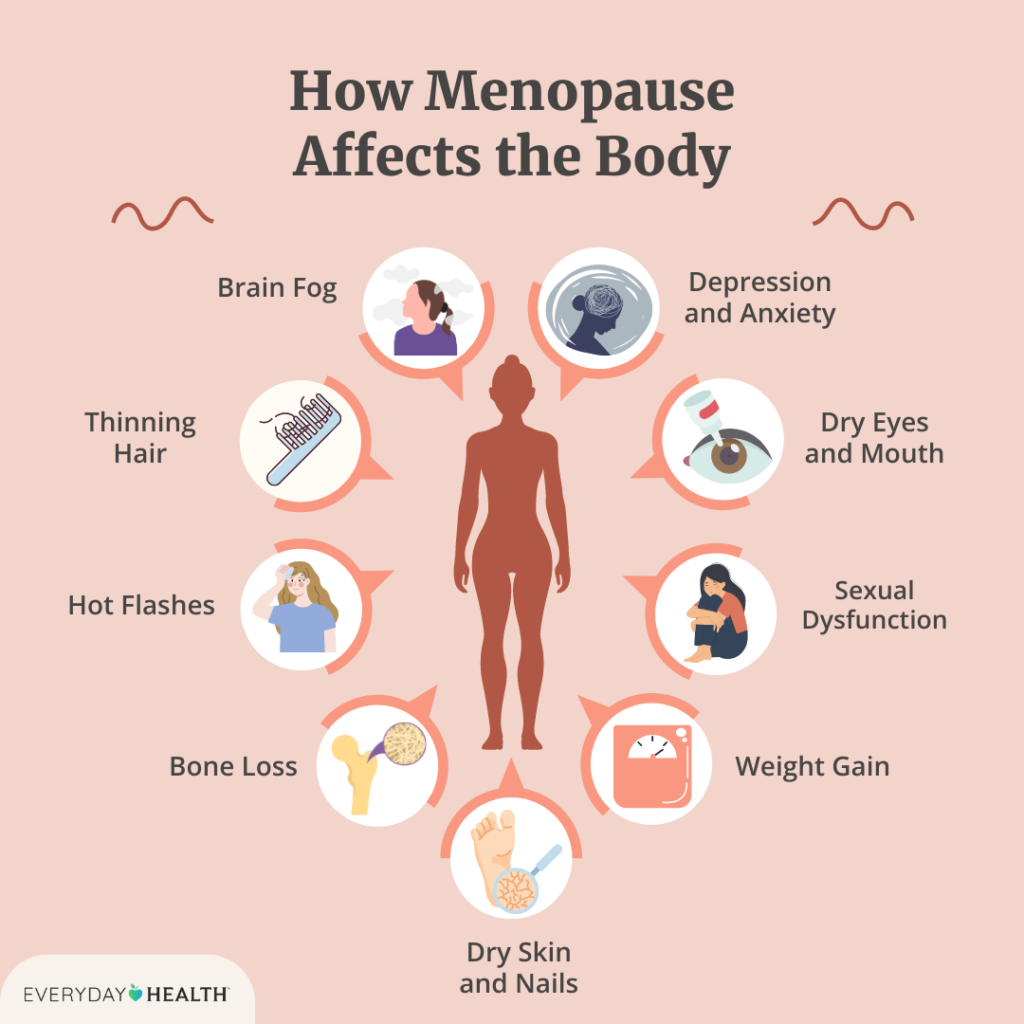
Some of the most common symptoms include:
➜ irregular periods (when periods come closer together or further apart), and when blood flow becomes lighter or heavier
➜ hot flushes
➜ night sweats
➜ headaches and migraines
➜ disturbed sleep patterns
➜ vaginal dryness
➜ joint pain
➜ fatigue
➜ short-term memory problems
➜ dry eyes
➜ dizziness
➜itchy or ‘creepy’ skin
➜ mood swings
➜ anxiety and irritability
➜lower libido or sex drive
➜ difficulty concentrating and making decisions
Hot flushes and night sweats
Up to 80% of people going through menopause experience hot flushes, but they tend to go away within one to two years. Common triggers for hot flushes are caffeine, alcohol, and spicy food. Traditional or natural remedies that are reported to be useful include a diet rich in legumes, grains, nuts and seeds, sage tea, black cohosh, or acupuncture.
Menopausal Hormone Therapy (MHT)
Adequate exercise, a healthy, balanced diet, taking time for rest and relaxation, and smoking cessation can all help address the symptoms of menopause.
For people who are struggling with menopausal symptoms, Menopausal Hormone Therapy (MHT) is available (this used to be known as Hormone Replacement Therapy, or HRT).
Healthify has more information about MHT, what it does, and the different ways of taking it. Talk to your healthcare provider or GP if your menopausal symptoms are affecting your quality of life, to see if MHT is right for your circumstances.
Myths and misunderstandings about MHT
There are several common myths and misunderstanding about Menopausal Hormone Therapy. Many of the myths about MHT come from the Women’s Health Initiative (WHI) studies of 2002 and 2004. More recent information about MHT means doctors better understand the risks and benefits of MHT. Whilst there are always risks involved when taking any medication, MHT is one of the best ways to control menopausal symptoms that are having a negative impact on your wellbeing.
Combined MHT (oestrogen plus progestogen) or oestrogen alone cause no significant increase in breast cancer or heart disease risk in women aged 50 to 59 or in women who start treatment within 10 years of menopause.
This factsheet from the Australian Menopause Society talks about 9 common myths and misunderstandings.
Useful links
Healthify NZ » More information about a range of Menopausal Hormone Therapy (MHT) topics
Menopause – Sexual Wellbeing Aotearoa » information on managing menopause in New Zealand
Menopause – Mayo Clinic » general information on menopause
NZ Early Menopause Support Group » support group for women in New Zealand experiencing early menopause
The Unspoken Truth About Menopause » watch this NZ Herald feature on menopause from 2024 on YouTube